NHS inefficiency has been a stumbling block for many a British government. Should ministers address head-on the near-infinite challenges plaguing a bloated and antiquated system? Or should they take the easier option, shuffling the data and redefining the terms, without tackling any of the underlying causes? Labour’s latest gambit, paying hospitals £3 million a month to remove patients from waiting lists, decisively falls into the latter camp.
Keir Starmer’s government has committed to ensuring that 92% of patients wait no longer than 18 weeks for elective care by the end of the parliament. By the 2024 general election, the waiting list stood at roughly 7.6 million people, nearly triple its level when the Conservatives entered office in 2010. What was once a routine measure of NHS throughput has therefore become the defining benchmark of health policy, and a proxy for the perceived competence of the British state itself.
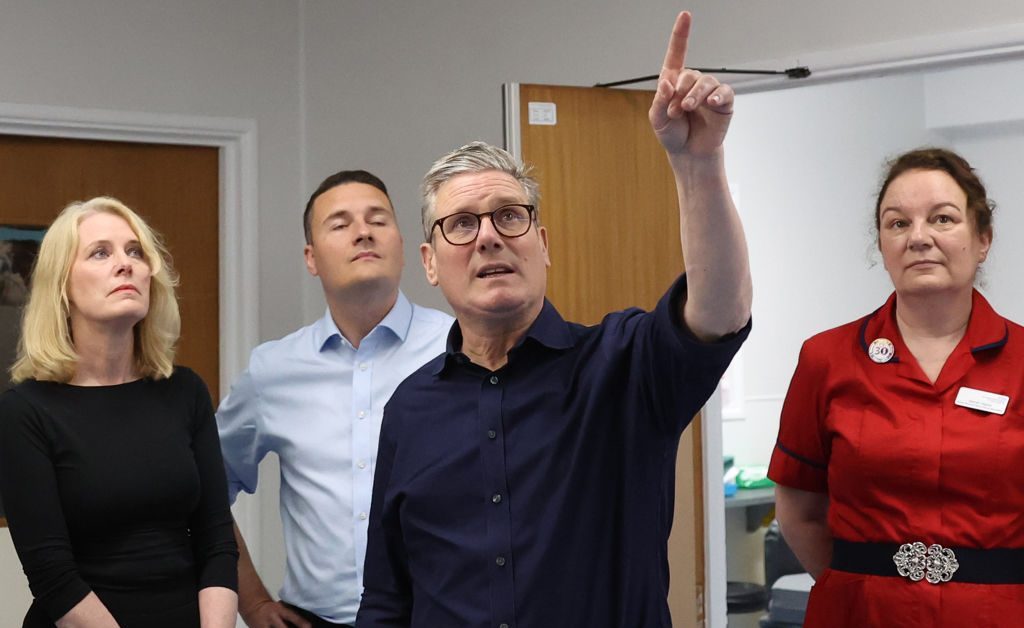
That reality has placed particular pressure on the Health Secretary, Wes Streeting, who has tied his political credibility to this single, highly visible target. He has pointed to an apparent drop by 86,000 patients in November, which is all the more impressive given that, over the same period, outpatient activity did not increase at all. On the contrary, NHS data show there were 10% fewer appointments than in October.
One is therefore forced to conclude that the Labour-run national healthcare system has stumbled upon a new golden age of productivity, in which waiting lists shrink without the inconvenience of patients actually being seen. The less miraculous explanation, of course, is “validation”: a standard administrative exercise to tidy up waiting lists, now turbocharged by the introduction of incentive payments for hospitals willing to carry it out.
This loophole, referred to as “Patient Not Present” activity, is designed to reward NHS trusts which identify and subsequently remove a patient who no longer needs to be seen in person. It provides cash-strapped hospitals with a payment of approximately £33 per patient removed from the waiting list through administrative means. Last year, hospital trusts received nearly £19 million for completing this validation process, equivalent to over half a million patients being removed from the waiting list without treatment. Consequently, there appears to be a chasm opening between the headline figures lauding falling backlogs and the clinical reality on the ground.
Such an approach risks masking a stagnation in the number of individuals actually receiving treatment, while simultaneously creating a perverse incentive to prioritise the opposite. Instead, policymakers must put aside performative governance measures that are steeped in short-termism, in order to address the layers upon layers of bureaucracy which have prevented the NHS from competing with the efficiency seen in the private sector. This will allow funding to be targeted in areas where real results can actually be delivered, rather than on-paper gains that do not correlate with patient experience.
For too long, politicians have been rewarded for avoiding hard work, eagerly focusing resources on any quick fix that will provide sufficient ammunition for their communication strategy. Yet, despite this gaming of metrics being far from a new phenomenon, the stakes are unquestionably higher when it enters the realm of healthcare.









Join the discussion
Join like minded readers that support our journalism by becoming a paid subscriber
To join the discussion in the comments, become a paid subscriber.
Join like minded readers that support our journalism, read unlimited articles and enjoy other subscriber-only benefits.
Subscribe