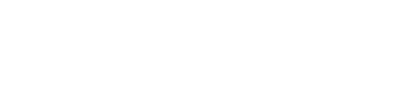
An LA production of 4.48 Psychosis. (Anne Cusack/Los Angeles Times via Getty Images)

The discovery of antipsychotics was an accidental revolution, the result not of systematic research, but of random observations. In the early Fifties, an obscure French naval surgeon was trying out chlorpromazine as a potential anaesthetic; he noticed that it calmed some of his patients. This inspired psychiatrists to try out the drug — there being virtually no constraints on pharmacological research in these years — and many reported that it functioned as a major tranquilliser. Before long, the company that owned the rights to the pill in North America had put it on the market. The dawn of psychopharmaceuticals had broken.
The psychiatric profession rapidly embraced the new pills, which more closely resembled the practices of mainstream medicine than the remedies that had previously been used to treat mental illness: insulin comas, shock treatments, lobotomies. Nobody really knew why the drugs worked. We still don’t, entirely. Serious mental illness is a source of profound suffering, and its ravages rapidly spill over to affect patients’ families, their immediate community, and society at large. This creates a desperation to do something — anything — to cope with its symptoms. Yet our understanding of the origins of psychosis remains strikingly primitive and feeble — and so, too, our understanding of its treatment.
Earlier this year, The Times reported that clozapine, a relative of chlorpromazine, is “Britain’s most dangerous prescription drug”. Prescribed in Britain to some 37,000 people suffering from schizophrenia each year, it has been associated, the story noted, with around 7,000 deaths since 1990: the equivalent of around 400 each year. There is a whiff of journalistic hyperbole at work here. A death rate of more than 1% of those taking the drug is certainly cause for concern, but there are far more dangerous drugs in the pharmacopoeia. Nevertheless, it is worth asking how clozapine ended up on the market, and why it continues to be prescribed.
The puzzles psychiatry wrestles with are so difficult to solve that when an intervention appears to work, enthusiasm tends to win out against any cautious restraint. So it was with the arrival of antipsychotics. Within 18 months of the first chlorpromazine pills being approved for the market, they were being prescribed to more than two million patients in the US. The now defunct pharmaceutical company Smith, Kline & French had bought the North American rights to the drug, but others were rushing to create their own copycat versions. In the words of an early advertisement for Thorazine: “Assaultive or destructive behaviour is rapidly controlled… helping to dispel or modify delusions, hallucinations and confusion, while keeping the patient calm and approachable.”
The drugs did indeed work, to a degree. They didn’t cure psychosis, but for many patients they alleviated some of its most dramatic and disturbing symptoms: the hallucinations and delusions that plagued them. Sadly — and this took years to be acknowledged — these medications had little effect on other devastating symptoms: the intellectual deterioration, the apathy, the failure to connect with others, the loss of spontaneity.
Early on, there were troublesome signs that the drugs imposed a heavy burden on those taking them: side-effects that surfaced and often persisted even after the drugs were withdrawn. Patients became incurably restless. They developed Parkinson’s-like symptoms. Most disturbing of all was a condition labelled tardive dyskinesia. A so-called extrapyramidal disorder, it involves facial tics, grimacing, grunting, rapid jerking and spasmodic movements — all of which are ironically often mistaken by naïve observers as symptoms of mental illness. It afflicts very many patients — estimates range as high as two-thirds of those taking the drugs — and is incurable, continuing even after people stop taking chlorpromazine.
For a decade and more, psychiatrists ignored this on-going iatrogenic disaster. Leading figures in the drugs revolution minimised its presence or significance. Nathan Kline, often called “the father of psychopharmacology” and once a serious candidate for a Nobel Prize in Medicine, insisted that tardive dyskinesia was “of no great clinical significance”. Daniel X. Freedman, the long-time editor of the Archives of Neurology and Psychiatry, claimed that the disorder was only found in a handful of patients, and was an “unavoidable price to be paid” for relief from delusions and hallucinations.
People wanted to believe chlorpromazine was a silver bullet; when you are confronted by the distressing symptoms of mental illness, it is tempting to ignore the drawbacks of anything that might offer relief. The current vogue for poorly researched and dubious interventions for sufferers of depression — deep brain stimulation, psychedelics, ketamine infusions — is only the latest example of this tendency.
But eventually the medical establishment couldn’t keep ignoring the dangers of chlorpromazine. A 1973 paper by Maryland psychiatrist George Crane, which appeared in the august pages of Science, effectively ended the silence surrounding tardive dyskinesia. By 1980, two other prominent psychiatrists spoke of the profession’s attitude to the issue having moved “from curiosity and mild concern to panic”. But once the period of denial came to an end, the absence of alternative treatments was glaringly obvious. This is where clozapine enters the story.
Clozapine was actually not a new drug at all. First synthesised in 1958 by a small Swiss company later absorbed by Sandoz, it was brought to the European market in the early Seventies, despite concerns about its propensity to provoke seizures and low blood pressure. A significant number of patients developed a serious, often fatal condition called agranulocytosis, where a dramatic loss of white blood cells wrecks a patient’s immune system and leaves them overwhelmingly vulnerable to infections. Before clozapine entered the American market — then, as now, the most lucrative market for pharmaceuticals — it was abruptly withdrawn from sale in Europe. For nearly two decades, it vanished from the scene.
But as concern about chlorpromazine’s side effects mounted, it occurred to Sandoz that clozapine could be brought back to life. With the caveat that patients given the drug would need to have their white cell counts carefully monitored, regulatory approval was soon forthcoming. Now, clozapine is prescribed in cases where other antipsychotics have failed — why it works is a mystery, but the evidence that it often does is solid. Nevertheless, common side effects include agitation, constipation, dizziness and fatigue, seizures and tremors, and serious weight gain. It is an intervention that should be sanctioned only in desperate cases.
Just as chlorpromazine’s discovery prompted rival drug companies to create a host of copycat drugs, so the re-emergence of clozapine prompted the development of a raft of new potions in the Nineties. Collectively known as second-generation antipsychotics — though their chemical structures often have little in common — these drugs seem less likely to provoke tardive dyskinesia, although a large study funded by the United States’ National Institute of Mental Health, rather than the drug companies, raised some doubts about the strength of the evidence for that claim. But these drugs remain no more effective at relieving hallucinations and delusions than their predecessors, and just as inefficacious at treating other symptoms of schizophrenia: the social withdrawal, the lack of interest in life, the intellectual deterioration and loss of linguistic capacity. A careful 2008 review in Nature found that they were no more than moderately effective in 41% of those treated (versus the 24% who responded positively to placebo), and the response to treatment declined over time. Second-generation antipsychotics are therefore important for those who do respond, but very far from curative; the authors of this particular study concluded that “there is much room for more efficacious compounds”.
Some studies have been more critical. Over time, second-generation antipsychotics provoke massive weight gain (10 or 20kg is not uncommon), and they are associated with heart disease and disorders of the metabolic system. Many of those taking these pills develop diabetes. So it’s unsurprising that one authoritative 2015 review in the Journal of Psychopharmacology concluded that “the [adverse effects] profiles of the newer antipsychotics are as worrying as the older equivalents for the patient’s long-term physical health”.
The danger is that the inappropriate prescription of these drugs will give psychiatry a bad name. That sector of society with little empathy for the psychically troubled — groups like the Scientologists or the followers of the late psychiatrist Thomas Szasz, who proclaimed that mental illness is a myth — will discuss side-effects in order to dismiss psychiatry as toxic or, worse, an “industry of death”. Patients who fail to respond to antipsychotics (and there are many), or who experience only the negative consequences of taking these pills, in many instances echo some of the complaints of these critics. I understand their anger and dismay. As a historian who has researched the foibles and failings of psychiatry, and the manifold ways its interventions have often served to magnify rather than reduce suffering, I’m not blind to the profession’s deficiencies.
But that very familiarity with the barbarities that often preceded the psychopharmacological revolution prompts me to a somewhat less bleak assessment of the profession’s current state. Before totally denigrating psychiatry, it is necessary to face up to the suffering and disruption that follows in the wake of mental illness. It is vital, I think, not to resort to nihilism. There are substantial numbers of people for whom drugs provide considerable relief. These pills permit many to live some semblance of a normal life.
All medical interventions carry risks, and balancing risks and harms is a problem for medicine as a whole, not just for psychiatry. Caution is especially in order in the psychiatric realm, precisely because the stigma that attaches to mental illness may encourage some to clutch at straws, and because psychiatric conditions cannot usually be cured. But caution and scepticism should not become despair. We’re talking about some of the most profound forms of human suffering. If our treatments are imperfect, we should simply attempt to do better.





Join the discussion
Join like minded readers that support our journalism by becoming a paid subscriber
To join the discussion in the comments, become a paid subscriber.
Join like minded readers that support our journalism, read unlimited articles and enjoy other subscriber-only benefits.
Subscribe